The Cost of Delivery Errors in Healthcare—and How to Prevent Them

In healthcare logistics, delivery accuracy is a non-negotiable requirement. A single error—whether it’s a misrouted specimen, delayed pharmaceutical, or misplaced medical device—can result in diagnostic delays, compromised patient safety, and regulatory non-compliance. These failures are not theoretical risks; they represent quantifiable costs and clinical consequences.
As healthcare systems adopt more complex logistics workflows across distributed care environments, preventing delivery errors is critical to maintaining continuity of care and operational integrity.

1. Clinical Consequences of Delivery Failures
Unlike general logistics, medical deliveries are tightly coupled with time-sensitive clinical workflows. A delayed pathology specimen can postpone a cancer diagnosis; a missed infusion delivery may disrupt a chemotherapy schedule. In home healthcare settings, the late arrival of respiratory devices or wound care kits can compromise patient outcomes and create liability exposure.
Direct Consequences Include:
- Diagnostic delays from lost or degraded specimens
- Treatment interruption due to unavailable medications
- Surgical cancellations from misrouted instruments or implants
- Breach of chain-of-custody in legal or transplant-related cases
2. Financial and Legal Implications
The cost of delivery errors extends beyond clinical setbacks. Repeat testing, rescheduling, and corrective logistics all drive up operational expenditures. If protected health information (PHI) is involved in a delivery breach, the incident may trigger HIPAA penalties and reputational damage.
In high-acuity cases, errors involving blood products, chemotherapy, or controlled substances can result in malpractice claims and regulatory scrutiny.
Key Cost Drivers:
- Recollection and retesting costs
- Overtime and rescheduling for clinical teams
- Fines related to HIPAA violations or DOT noncompliance
- Litigation and settlement costs from patient harm
3. Common Root Causes of Medical Delivery Errors
Medical delivery errors frequently stem from systemic gaps rather than isolated mistakes. These may include insufficient chain-of-custody tracking, lack of temperature control, inconsistent labeling, or miscommunication between logistics and clinical teams.
Typical Error Points:
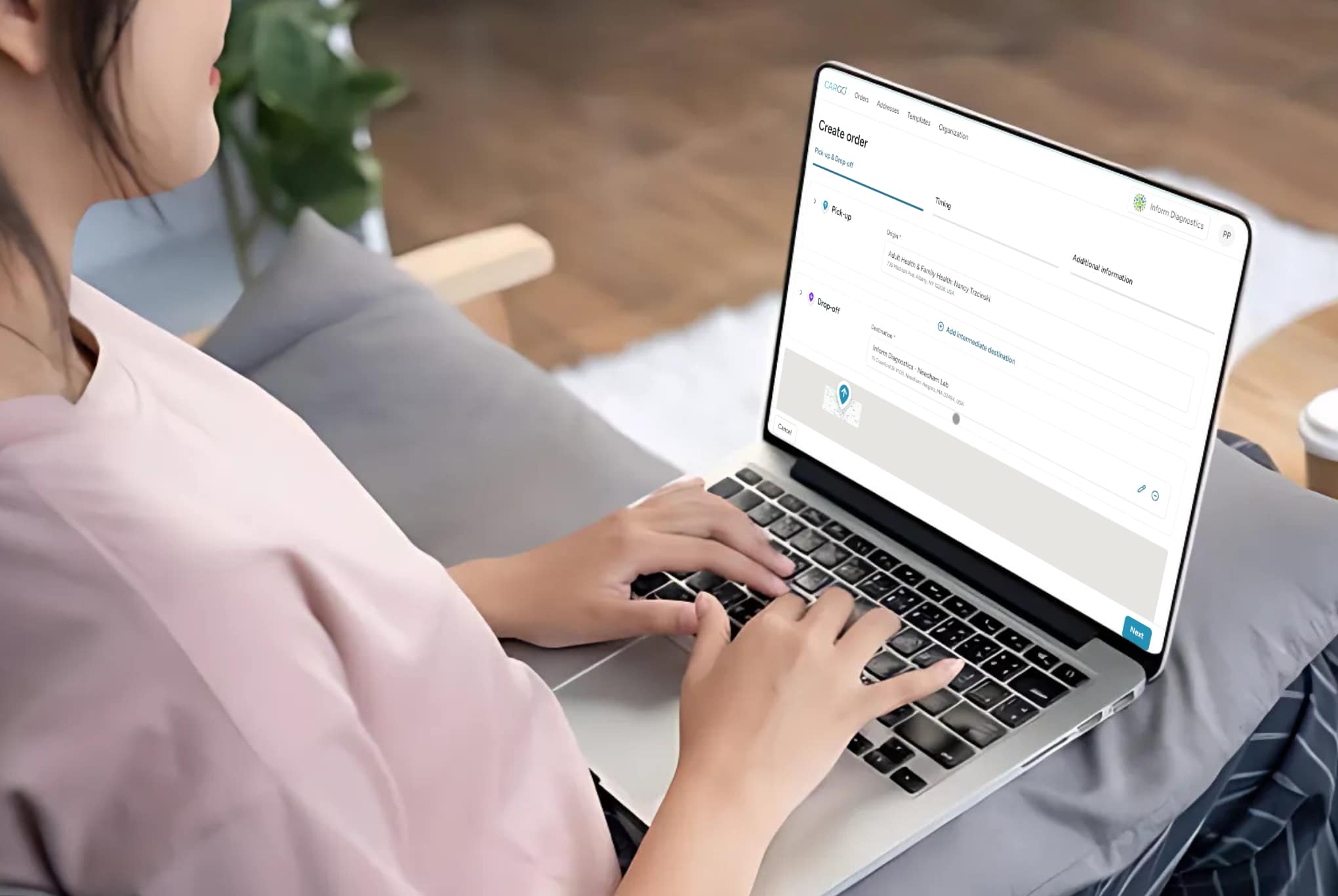
- Manual entry mistakes in pickup/drop-off instructions
- Inadequate packaging for temperature-sensitive materials
- Lack of real-time tracking or milestone alerts
- Poorly trained couriers unfamiliar with healthcare protocols
4. Quality Control Measures for Error Prevention
A logistics quality control framework is essential to minimize risks. This includes standardized courier training, barcode-based specimen identification, automated dispatch systems, and continuous chain-of-custody documentation.
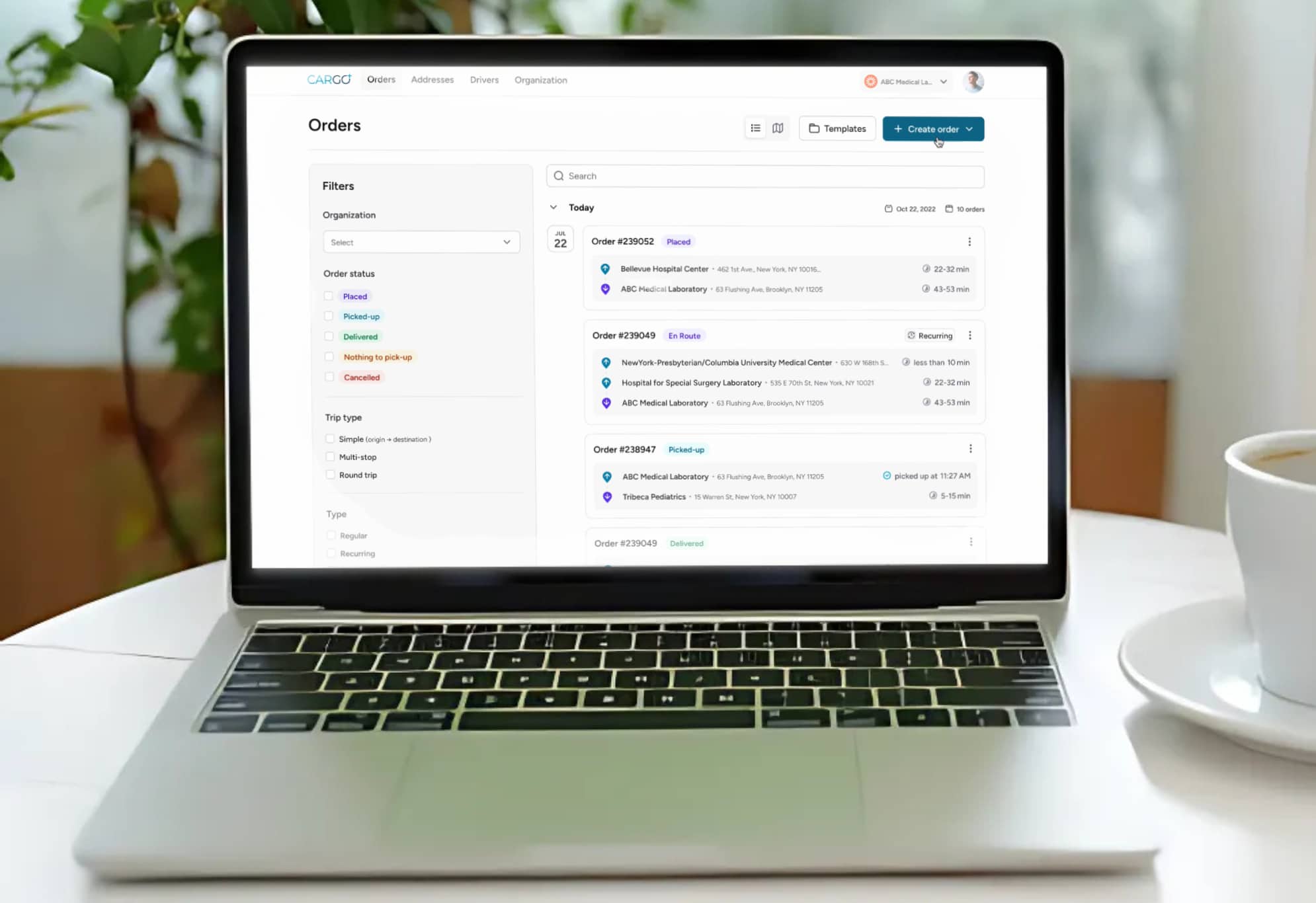
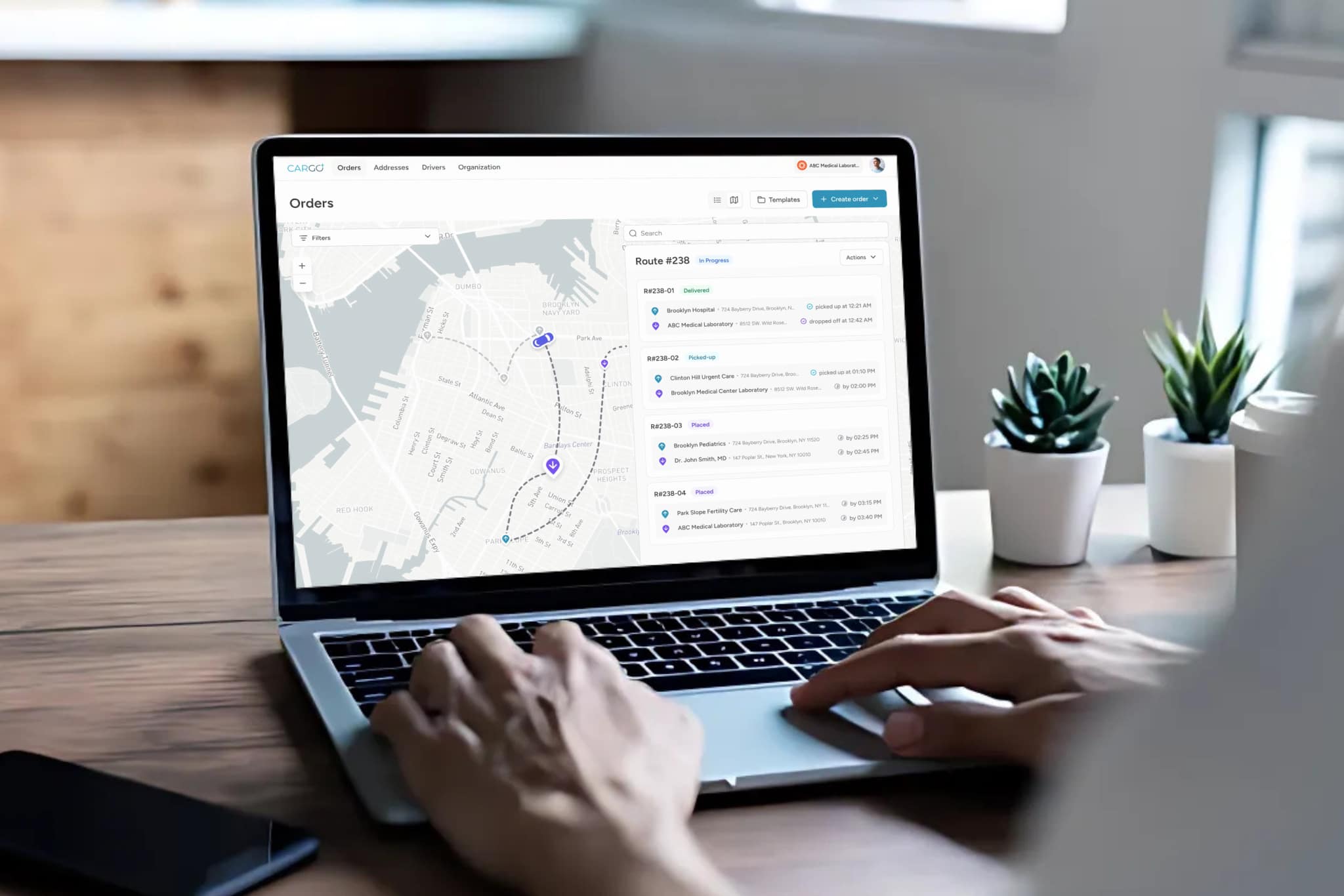
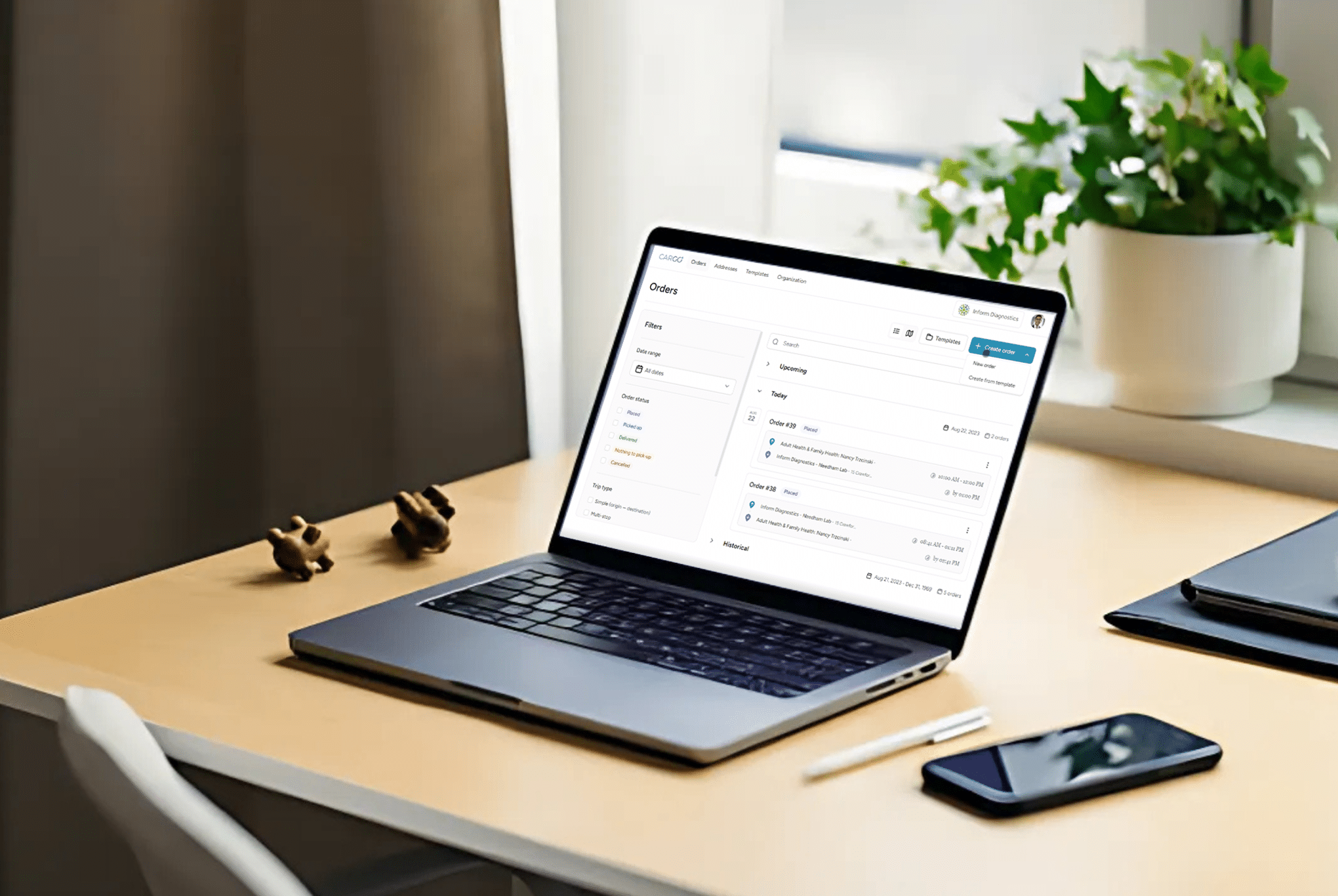
Real-time tracking software with exception alerting allows clinical teams to respond proactively when a delivery deviates from its expected path. Quality audits, SLA monitoring, and issue resolution workflows should be embedded into the courier process.
Effective Prevention Practices:
- Digital order verification and tracking
- Electronic proof-of-delivery with geotags and timestamps
- Packaging protocols for fragile or regulated materials
- Real-time alerting for temperature excursions or route deviations
5. Building a Culture of Delivery Accountability
While technology is a critical enabler, process discipline and organizational alignment are equally important. Healthcare providers should treat delivery partners as extensions of clinical operations, with shared KPIs and quality benchmarks.
Incident reviews, root cause analysis, and continuous improvement cycles should be conducted jointly between courier providers and healthcare logistics coordinators. This creates a feedback loop that reduces variability and raises performance standards.
Organizational Practices Include:
- Joint SLA performance reviews
- Courier credentialing and compliance audits
- Integration of logistics metrics into patient safety initiatives
Final Thoughts
Medical delivery errors carry costs that reach far beyond the logistical realm—they can disrupt care, endanger patients, and compromise compliance. Preventing these failures requires a combination of process rigor, specialized courier capabilities, and integrated technology. For healthcare providers, investing in logistics quality control is both a clinical responsibility and a strategic imperative.