What to Look for in a HIPAA-Compliant Medical Courier

As healthcare delivery expands beyond clinical facilities into homes, labs, and decentralized care models, the integrity and confidentiality of protected health information (PHI) during transport has never been more critical. Medical courier services that claim HIPAA compliance must meet stringent technical, administrative, and procedural safeguards to protect sensitive data.
Healthcare organizations that engage third-party logistics providers for specimen transport, medication delivery, or medical equipment must ensure that these vendors meet all HIPAA requirements—not just in letter, but in daily operational practice.

1. Proven Security Protocols and Training
HIPAA compliance is not achieved by default—it is implemented through formalized protocols and consistent workforce training. A HIPAA-compliant medical courier must maintain strict access controls, ensure driver background checks, and conduct regular workforce education on PHI handling.
Each courier should be trained in identifying and mitigating risks such as package tampering, lost documentation, or unauthorized disclosure. Personal devices, if used, must be encrypted, and access to PHI must be restricted to authorized personnel only.
Key Elements:
- Documented HIPAA training for all drivers
- Controlled access to packages with PHI
- Background screening and confidentiality agreements
2. Chain-of-Custody Integrity
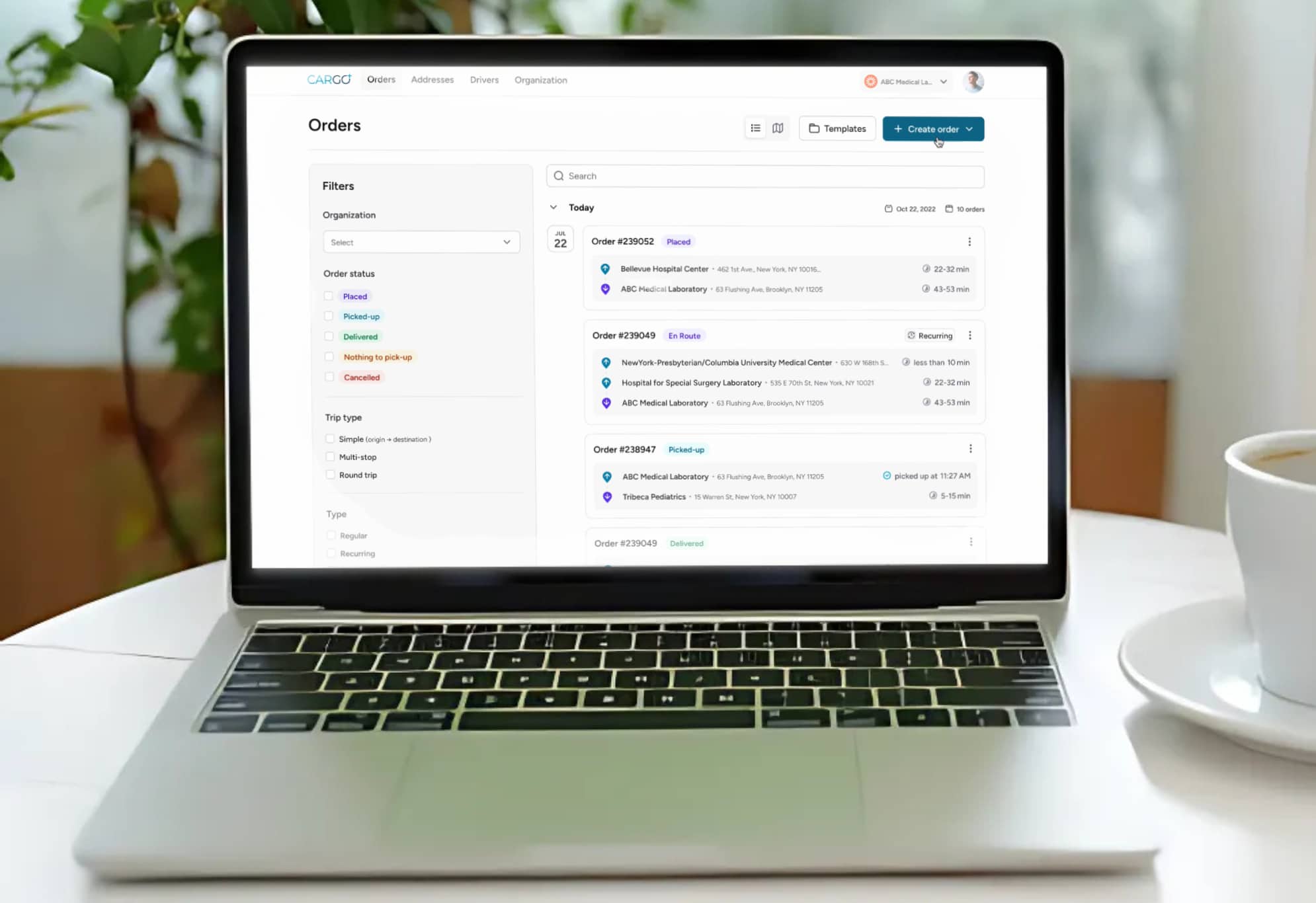
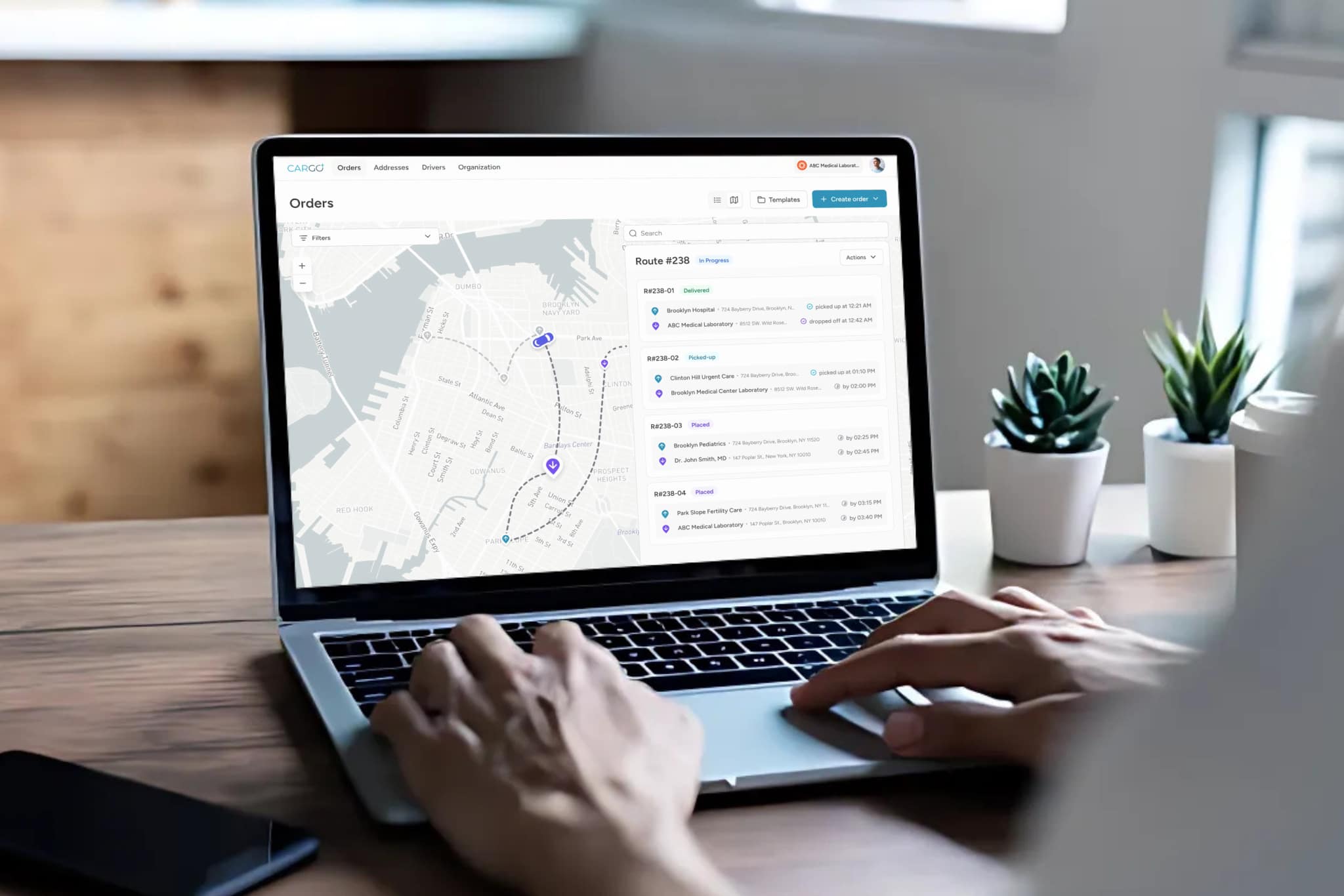
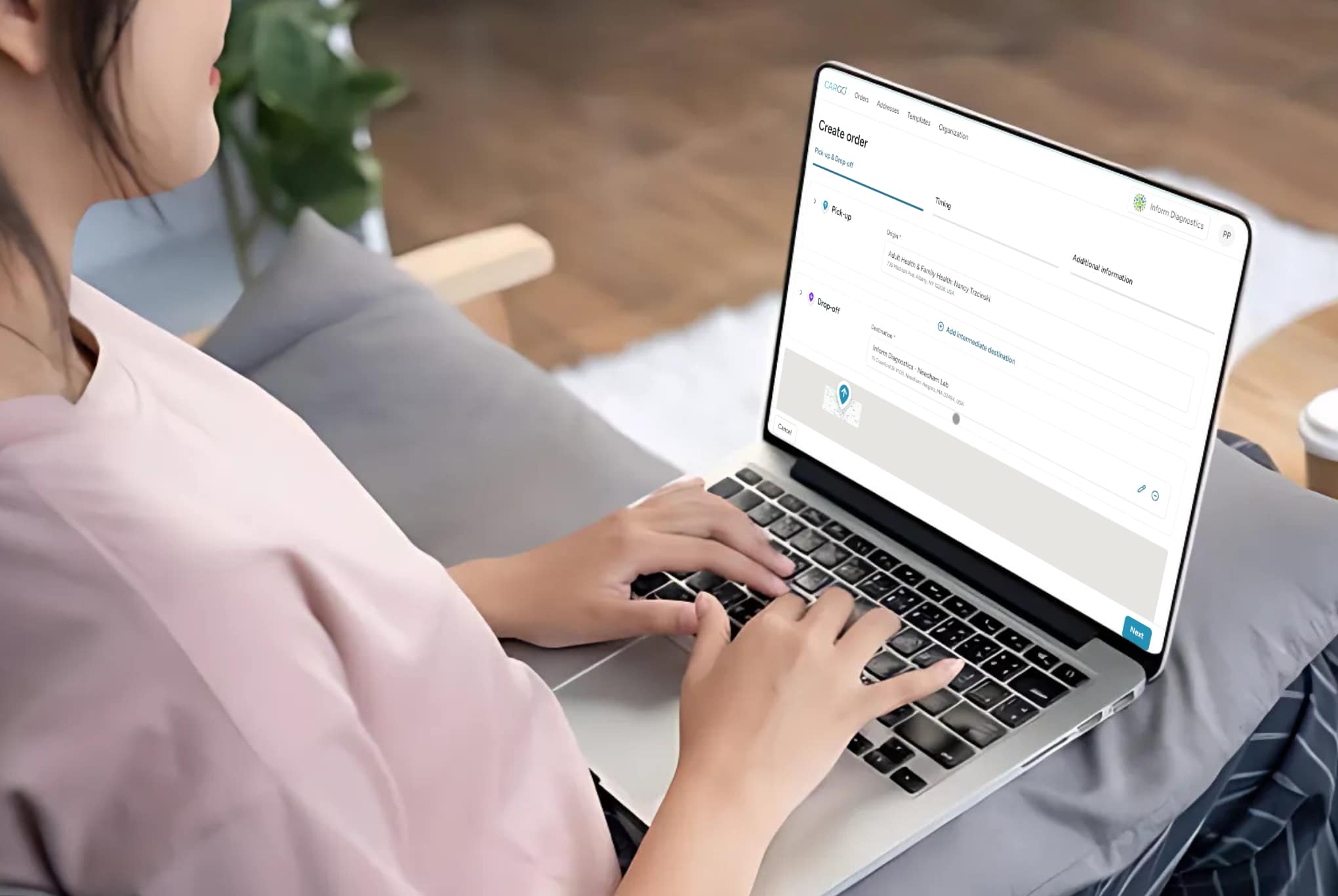
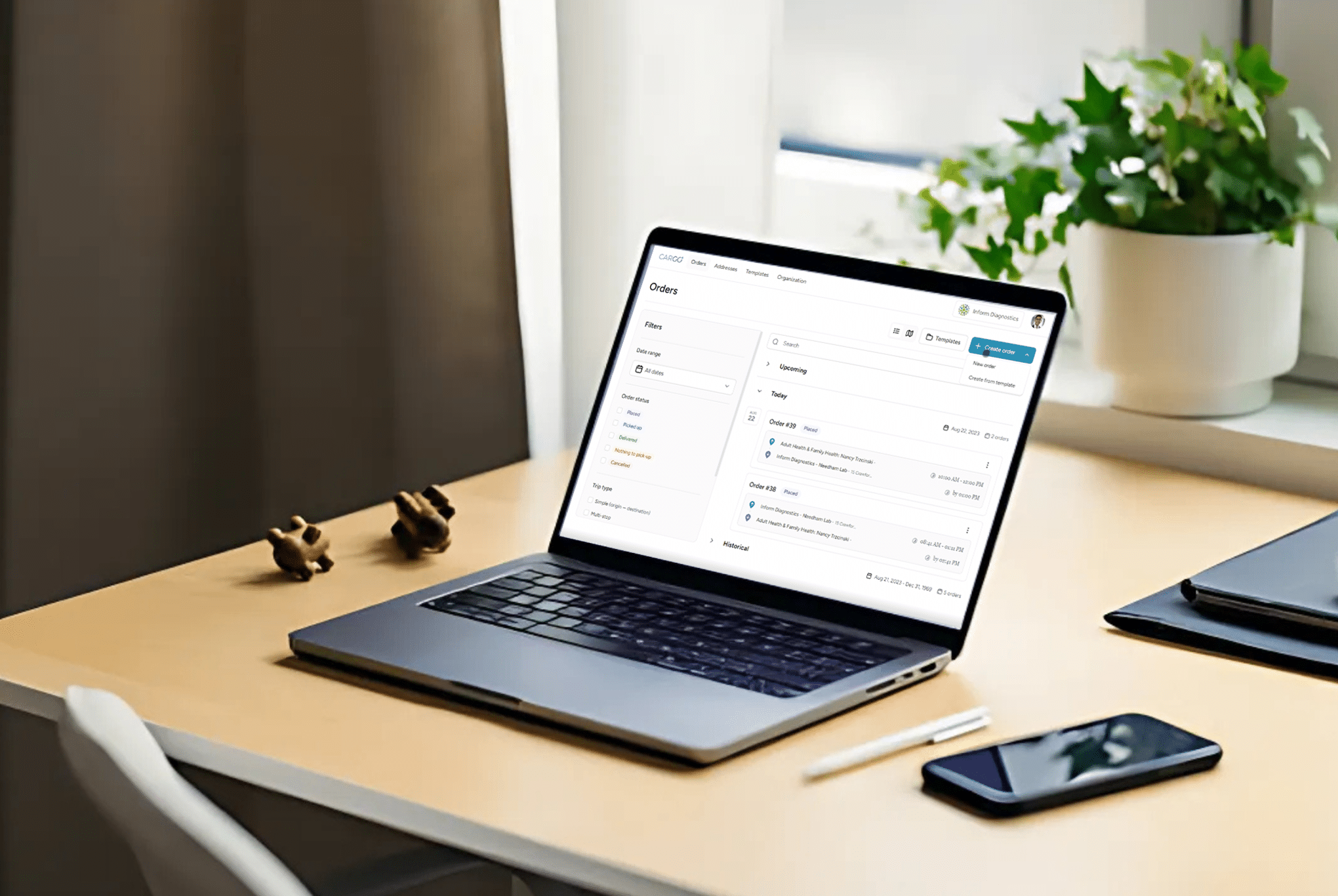
Maintaining an unbroken, auditable chain of custody is essential for both compliance and operational transparency. A qualified courier should provide timestamped pick-up and drop-off logs, digital signatures, and documentation of every handoff or route deviation.
This is especially vital for time-sensitive specimens, diagnostic samples, and prescription medications, where the loss of traceability can impact clinical outcomes and trigger compliance violations.
Chain-of-Custody Features:
- Digital documentation of all handoffs
- Real-time tracking with route history
- Secure electronic signature capture
3. Encrypted Communication and Technology Infrastructure
HIPAA requires that any electronic PHI (ePHI) transmitted or stored by a third-party provider be encrypted and securely maintained. Look for courier platforms that use HTTPS, data-at-rest encryption, and endpoint security controls.
Route optimization systems, delivery status updates, and EHR integrations must all be built with a focus on information security. Alerts or messages containing PHI should never be transmitted via unsecure SMS or email.
Technology Safeguards Should Include:
- TLS/SSL encryption for web and mobile platforms
- Secure APIs for integration with healthcare systems
- Audit logs and access controls for digital tools
4. Incident Response and Breach Notification Procedures
Even the most secure systems can encounter anomalies. A reliable HIPAA-compliant courier should have a documented incident response plan, with predefined protocols for breach identification, containment, reporting, and corrective action.
Healthcare providers are ultimately accountable for vendor missteps under HIPAA’s Omnibus Rule. Therefore, the presence of a formal response framework is not optional—it is a core requirement.
Best Practices Include:
- Written breach notification policies
- Defined timelines for incident reporting
- Root cause analysis and mitigation planning
5. Business Associate Agreement (BAA)
No engagement with a HIPAA-covered entity is valid without a signed Business Associate Agreement. This legal document outlines the courier’s responsibilities in protecting PHI and establishes liability terms in the event of noncompliance or breach.
Ensure the BAA covers all areas of potential exposure, including subcontractors, mobile apps, cloud storage vendors, and customer support processes.
BAA Essentials:
- Scope of PHI access and permitted uses
- Breach response commitments
- Data retention and disposal policies
Final Thoughts
Selecting a HIPAA-compliant medical courier is not simply a logistical decision—it is a strategic compliance obligation. Healthcare organizations must verify that any transport provider they engage can document security controls, enforce disciplined chain-of-custody processes, and integrate with the broader framework of data protection.
The cost of noncompliance is measured not only in penalties, but in patient trust, diagnostic accuracy, and operational reliability. In this context, due diligence is both a regulatory necessity and a clinical imperative.